Looking for a heart transplant in Delhi? We know a heart transplant is a big decision. It’s more than just surgery, it’s a chance for a new lease on life. That’s why our team of highly skilled heart specialists, surgeons, and caregivers is dedicated to providing exceptional care every step of the way.
We use the latest technology and our extensive experience to create personalized treatment plans for each patient. Our goal is to not only heal your heart but also to improve your overall quality of life after the transplant. This commitment makes Ayushman Hospital one of the leading heart transplant centers in Delhi, India.
What is a Heart Transplant?
A heart transplant involves surgically replacing a diseased heart with a healthy one obtained from a donor. This operation is usually performed for people with severe heart failure or coronary artery disease when other treatments haven’t worked. It’s a major surgery, but it can be a life-saving option for people who are very sick.
Is a heart transplant in Delhi right for me?
A heart transplant is a major surgery considered when all other treatments have failed. Doctors recommend it for patients with severe heart failure where their heart can’t pump blood effectively anymore. This surgery offers a chance for a longer and improved life, but it’s important to explore all options with your doctor first.
What can cause heart failure?
Heart failure arises when the heart inadequately pumps blood. Presented below are some key contributing factors:
- Weakened Heart Muscles: This can be caused by a condition called dilated cardiomyopathy, where the heart muscle becomes enlarged, thickened, or stiff.
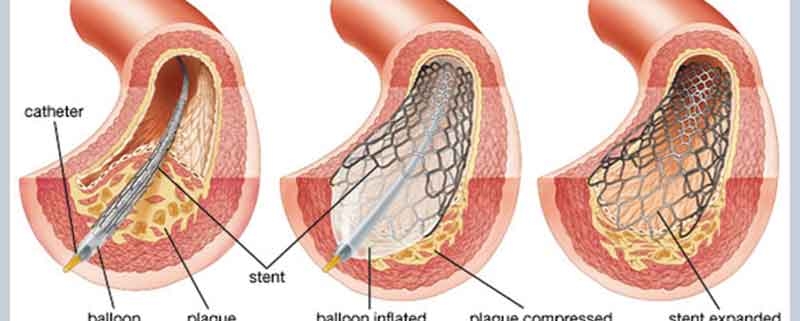
- Severe Coronary Artery Disease: When plaque builds up in your arteries and damages your heart tissue, it can lead to severe coronary artery disease and eventual heart failure.
- Birth Defects: Some people are born with heart abnormalities that can’t be fully corrected with regular surgery. These may require a heart transplant or even a combined heart and lung transplant.
- Valve Problems: If one of your heart valves is damaged or defective (valvular heart disease), it can interfere with blood flow and contribute to heart failure.
- Previous Transplant Failure: In rare cases, a previously transplanted heart might not function properly anymore, necessitating another transplant.
Who can get a heart transplant?
A heart transplant is a life-saving option for people with severe heart failure, but it’s not for everyone. Here’s why a careful evaluation process is crucial:
- Severity of Illness: This surgery is typically considered a last resort for people whose heart is failing so badly that other treatments haven’t worked.
- Overall Health: Doctors will assess the health of all your organs to make sure they’re strong enough to handle the transplant and recovery.
- Cancer and Infections: Active cancer or serious infections can increase the risk of complications after surgery.
- Lifestyle Choices: Smoking, heavy drinking, and uncontrolled diabetes can significantly impact the success of a transplant. These habits put extra strain on a new heart.
If you meet these initial criteria, further evaluation follows. Patients who continue to smoke or have poorly managed diabetes may not be eligible. Ultimately, if you’re deemed a good candidate, your name will be added to the national waiting list for a donor’s heart.
The Wait for a New Heart
The wait for a donor’s heart can vary depending on several factors. There’s no set timeframe because hearts are matched based on compatibility, not on a first-come, first-served basis. Here’s what affects the waiting time:
- Compatibility: Matching blood type, organ size, and minimizing antibody rejection are crucial.
- Waiting List Position: How long you’ve been waiting plays a role, but it’s balanced with the urgency of your condition.
- Your Health: Staying as healthy as possible while you wait improves your chances of a successful transplant.
While waiting, it’s important to focus on maintaining your health. This might include following a specific diet, taking medications as prescribed, and exercising when possible (according to your doctor’s guidance).
Heart Transplant Surgery Procedure
When a matching donor heart becomes available, time is of the essence! The transplant surgery needs to happen within 4 hours of the heart being removed from the donor. As soon as you’re notified by Ayushman Hospital, it’s important to act quickly to proceed with the surgery.
It’s important to understand that getting a heart transplant in Delhi, India is a multi-step process. The initial evaluation and preparation happen well before the actual surgery. Here at Ayushman Hospital, our team of highly skilled heart transplant surgeons will guide you through every step of the way.
What to Expect During Heart Transplant Surgery
A heart transplant in Delhi is a major surgery, typically lasting 4-6 hours. If you’ve had previous heart surgeries or complications arise, it might take longer. Here’s a general outline of what to expect:
- Chest Access: The surgeon will make an incision in your chest to access your heart.
- Heart-Lung Bypass: A special machine will temporarily take over the job of your heart and lungs, keeping oxygen-rich blood flowing throughout your body.
- Heart Removal: Once the bypass machine is working, your own heart will be carefully removed.
- Donor Heart Placement: The donor’s healthy heart will be stitched into place and connected to your blood vessels.
- Restarting the Heart: Ideally, the new heart will begin beating on its own once blood flow is restored. In some cases, a gentle electrical shock might be used to stimulate the heart.
- Recovery: After surgery, you’ll be on a ventilator and closely monitored until your condition stabilizes. This may take several days in the Intensive Care Unit (ICU).
Remember, this is a general overview. Your doctor will explain the specifics of your surgery in more detail.
Recovery After Your Heart Transplant
After a successful heart transplant, you’ll be closely monitored in the hospital for several weeks. This allows doctors to ensure your body is adjusting well to the new heart. During this time, expect regular tests like heart biopsies, EKGs, echos, and lung function tests to track your progress.
Here are some key things to know about recovery:
- Medications: You’ll take various medications to manage your health. One crucial type is immunosuppressants, which prevent your body from rejecting the donor’s heart. These medications can have side effects, so talk to your doctor about managing them.
- Rehabilitation: A personalized rehab program will help you adjust to your new lifestyle. This might include a heart-healthy diet and exercise plan to promote a strong recovery. Your cardiac rehab team will guide you through these changes.
- Emotional Support: It’s normal to experience a range of emotions after a major surgery like this.
Remember, a heart transplant offers a chance for a renewed life. By following your doctor’s instructions and focusing on healthy habits, you can optimize your recovery and enjoy a brighter future.
Why Choose Ayushman Hospital for Your Heart Transplant?
If you’re considering a heart transplant in Delhi, Ayushman Hospital can be your partner in this life-changing journey. Here’s what sets us apart:
- Expert Heart Transplant Team: Our surgeons are highly skilled and experienced, with a proven track record of success in complex heart transplant procedures.
- Advanced Technology: We are equipped with cutting-edge facilities, including a dedicated heart transplant unit and the latest medical technology to ensure optimal outcomes.
- Focus on You: We prioritize comprehensive patient care, providing support and guidance throughout the entire transplant process, from pre-surgery evaluation to post-operative rehabilitation.
- Trusted Reputation: Ayushman Hospital has earned a strong reputation for excellence in cardiac care, giving you peace of mind when making this crucial decision.
- Convenient Locations: With multiple locations across India, we strive to make critical care accessible to a wider range of patients.
We understand that a heart transplant is a major step. At Ayushman Hospital, we’re dedicated to providing you with the expertise, technology, and compassionate care you need for a successful outcome and a brighter future.